Plantar callus is a common yet often overlooked foot condition that develops as a protective response to repetitive pressure and friction on the soles, particularly over weight-bearing areas like the heels and balls of the feet. Understanding the causes, such as improper footwear, high arches, flat feet, or prolonged walking on hard surfaces, is crucial to addressing not only the callus itself but also the underlying factors that contribute to its formation. This guide not only equips you with practical solutions but also emphasizes long-term foot care strategies, encouraging you to read further for detailed methods, expert advice, and preventative tips to maintain healthy, comfortable feet.
plantar callus treatment
Plantar callus treatment focuses on reducing excessive pressure and friction on the sole of the foot while gradually removing thickened skin in a safe, evidence-based way. In clinical practice, effective plantar callus treatment begins with identifying biomechanical causes such as abnormal gait, high plantar pressure points, flat feet, or ill-fitting footwear, as these factors stimulate hyperkeratosis and skin cell overproduction. Conservative management includes regular mechanical debridement by a podiatrist, combined with keratolytic agents like urea, salicylic acid, or lactic acid that soften the stratum corneum and improve skin turnover. Treating calluses on the soles of the feet improves significantly when daily routines include proper hygiene, moisturizing, and pressure offloading as part of a consistent Foot care approach.
-
Formulation: Rich, emollient cream for intensive treatment
-
Target Condition: Dry feet, cracked heels, and calluses
-
Key Action: Intensive hydration, repairing of cracks, and softening of hardened skin.
Foot Cream
Plantar callus treatment also benefits from preventive strategies that address long-term foot health rather than just symptom relief, especially for older adults and individuals with diabetes or circulatory concerns. Custom orthotics, shock-absorbing insoles, and supportive footwear help redistribute plantar load and significantly lower the risk of recurrent plantar callus formation. Evidence shows that maintaining adequate skin hydration, avoiding aggressive home cutting, and managing contributing conditions such as obesity or joint deformities improves treatment outcomes. In Canadian clinical guidelines, patient education plays a key role, emphasizing routine foot inspection, proper hygiene, and early intervention to prevent complications like fissures, pain, or secondary infection.
How do you treat a plantar callus?
Treatment plantar callus starts by safely reducing the thickened skin and addressing the mechanical stress that caused it in the first place, as repeated pressure is the primary trigger for Plantar callus formation. From a clinical standpoint, podiatrists often recommend professional debridement to remove excess keratin, followed by topical keratolytic agents such as urea or salicylic acid to soften the stratum corneum and normalize skin cell turnover. Supporting the skin barrier with medical-grade moisturizers helps prevent cracking, while avoiding aggressive self-cutting reduces the risk of infection or tissue damage.

Treatment plantar callus focuses on prevention through pressure redistribution and foot biomechanics correction, especially for people who stand for long hours or have structural foot issues. Using cushioned insoles, custom orthotics, and properly fitted footwear lowers plantar pressure and minimizes recurrence of Plantar callus. Evidence-based foot health guidelines in Canada also emphasize regular foot inspections, maintaining adequate hydration of the skin, and managing contributing factors such as excess body weight or abnormal gait patterns to achieve lasting relief and improved mobility.
Plantar callus removal
Plantar callus removal is a targeted clinical process aimed at safely eliminating thickened skin while preserving the integrity of healthy tissue underneath, especially in weight-bearing areas of the foot. Medically supervised plantar callus removal typically involves sterile mechanical debridement performed by a podiatrist, which reduces hyperkeratotic layers caused by prolonged pressure and friction. This approach is often combined with topical keratolytic agents such as urea or salicylic acid that break down excess keratin and improve epidermal turnover. From a scientific perspective, controlled removal helps restore normal skin biomechanics, reduces localized inflammation, and alleviates pain associated with altered plantar pressure distribution.
Plantar callus removal should always be paired with preventive strategies to minimize recurrence and support long-term foot health, particularly for individuals with diabetes, circulatory disorders, or biomechanical abnormalities. Due to the effect of diabetes on the skin and hair, people with diabetes need to take extra care. Extra attention to hydration, gentle cleansing, and regular skin and foot checks is essential to maintain barrier function and overall skin health.
Evidence-based care emphasizes pressure offloading through custom orthotics, shock-absorbing insoles, and properly fitted footwear to reduce stress on the plantar surface. In Canadian foot care practice, patient education is considered essential, highlighting the importance of regular foot inspections, proper hydration of the skin barrier, and avoiding unsafe at-home cutting methods that may lead to infection or skin breakdown.
Plantar callus on heel develops when repeated pressure and friction on the heel cause the skin to thicken as a protective response, a process known medically as hyperkeratosis. This condition is common in people who stand or walk for long periods, wear poorly cushioned footwear, or have biomechanical issues such as heel fat pad atrophy or abnormal gait. From a clinical perspective, a plantar callus on heel can lead to discomfort, reduced shock absorption, and an increased risk of skin fissures if left untreated, especially in dry or cold Canadian climates where skin dehydration is more pronounced.
Plantar callus pain
Plantar callus pain occurs when excessive thickened skin on the sole of the foot begins to compress underlying tissues and nerve endings, often due to sustained pressure, friction, or altered foot biomechanics. Clinically, this pain is linked to hyperkeratosis that disrupts normal shock absorption, making everyday activities like walking or standing uncomfortable. Factors such as prolonged standing, improper footwear, high plantar pressure zones, and age-related fat pad thinning can intensify symptoms, while Plantar callus buildup may also increase localized inflammation and sensitivity in weight-bearing areas.
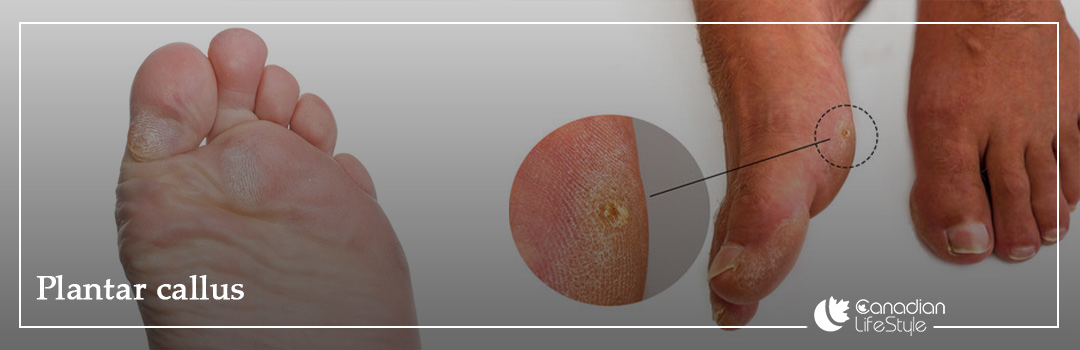
Plantar callus photos
Plantar callus photos serve as visual references to differentiate callus from related lesions such as corns, warts, or diabetic ulcers, aiding in accurate assessment and patient education about skin changes. When reviewing such photos, it’s important to notice patterns of hyperkeratosis and anatomical location, as these visual cues help clinicians tailor treatment plans and monitor progression or resolution over time.
Will a plantar callus go away on its own?
Generally, plantar calluses do not resolve without intervention because they develop as a protective response to chronic pressure or friction, leading to thickened skin layers that persist until the mechanical stress is addressed. Scientific observations suggest that even mild calluses may gradually worsen, potentially causing pain, fissures, or secondary infections if left untreated. Effective self-care, including pressure relief, cushioned footwear, and regular moisturization, is essential to prevent progression, while professional assessment ensures safe removal and long-term prevention.
What causes callus on the bottom of the feet?
Calluses form due to repetitive friction, pressure, or shear forces on the plantar surface, which trigger the skin to thicken as a protective mechanism. Biomechanical factors such as abnormal gait, high arches, flat feet, or improperly fitted footwear contribute significantly, concentrating stress on specific areas like the heels, balls of the feet, or toes. Over time, the epidermis responds with hyperkeratosis, producing a dense layer of keratin that appears as a plantar callus and may cause discomfort or pain if left unmanaged.
Is walking good or bad for foot calluses?
Is walking good or bad for foot calluses? Walking can have both positive and negative effects on plantar calluses depending on intensity, footwear, and existing foot structure. Moderate walking with properly cushioned shoes can improve circulation, maintain skin flexibility, and prevent excessive pressure buildup, which may help reduce callus formation over time. However, prolonged walking on hard surfaces, wearing ill-fitting shoes, or high-impact activity can exacerbate friction and pressure, worsening hyperkeratosis and potentially leading to pain or fissures in the plantar callus. Considering the Effect of Exercise on Skin, it is better to walk slowly and with the advice of a doctor.
What do podiatrists use to remove calluses?
Podiatrists commonly employ specialized instruments such as scalpels, curettes, and micro‑planing tools to carefully pare down thickened plantar skin while preserving underlying healthy tissue. This controlled mechanical debridement, often combined with keratolytic agents like salicylic acid or urea-based creams, softens the hyperkeratotic layer and allows for safe, gradual removal. Clinicians may also recommend orthotic inserts or cushioning to redistribute pressure and prevent recurrence of plantar calluses.
Read more: Causes and treatments for bad body odor
What might your foot callus be telling you?
A plantar callus often signals that your feet are under abnormal or excessive pressure, highlighting areas where your gait, footwear, or foot structure may be causing repeated friction. Scientifically, calluses act as the skin’s protective response to mechanical stress, but their presence can also indicate biomechanical issues such as high arches, flat feet, bunions, or uneven weight distribution. Observing the location, thickness, and shape of a callus provides valuable insight into which parts of the foot require offloading, cushioning, or professional intervention to prevent pain, fissures, or more serious complications.
How to get rid of hard calluses under feet?
Getting rid of hard calluses under feet involves a combination of safe mechanical removal and ongoing skin care to reduce thickness and prevent recurrence. Clinically, controlled parking using a pumice stone or a podiatrist’s scalpel can gradually reduce the hardened keratin layer, while keratolytic agents such as urea or salicylic acid soften the skin for easier exfoliation. Complementary measures like wearing cushioned shoes, using silicone or foam pads, and redistributing pressure with orthotic inserts address the underlying mechanical stress that caused the plantar callus.
How to remove callus on bottom of foot?
removing callus on the bottom of foot begins with reducing the thickened skin safely while addressing the pressure that caused it. For more persistent or painful calluses, podiatrists use precise debridement with a scalpel and may recommend keratolytic creams containing urea or salicylic acid to soften the skin. Coupling these treatments with cushioned footwear or custom orthotics helps redistribute pressure, preventing recurrence and supporting long-term foot health.
Should you remove calluses from the bottom of your feet?
Yes, but with caution, as plantar calluses serve as a protective barrier against repeated pressure and friction. Safe removal, ideally performed by a podiatrist or using gentle at-home methods like soaking and careful exfoliation, helps relieve discomfort and prevent cracking or infection without damaging healthy skin. Regular monitoring, moisturizing, and pressure redistribution through cushioned footwear or orthotics are essential to maintain foot health and prevent the callus from returning. If the callus is severe and the cracks are deep, use specialized care products and ignore home remedies.
Conclusion
In conclusion, plantar calluses are a common foot concern that reflect the skin’s natural response to repetitive pressure, friction, or biomechanical stress. Effective management involves a combination of proper foot care, safe mechanical removal, keratolytic treatments, and preventative strategies such as cushioned footwear, orthotic inserts, and daily monitoring. Understanding the causes, symptoms, and treatment options—including advice from podiatrists—helps reduce pain, prevent complications, and maintain healthy, resilient soles. By addressing both the existing callus and the underlying mechanical factors, individuals can protect their feet, improve comfort during walking, and support long-term foot health. Get our specialized products to treat and prevent calluses for better and faster results.